How Selerix Helps
Complex benefits challenges deserve clear, effective solutions. We help HR teams solve common benefits challenges— from enrollment to reporting and beyond.


You Don’t Have to Tackle Benefits Challenges Alone
Benefits have never been more complex, and employees have never expected more from them. From compliance to communication, HR teams are juggling it all, often without the tools or time to do it well.
That’s where Selerix comes in. We help thousands of employers take control of their benefits strategy and deliver a better benefits experience across the board.
Explore the common benefits challenges below — and discover how we help teams like yours stay ahead.
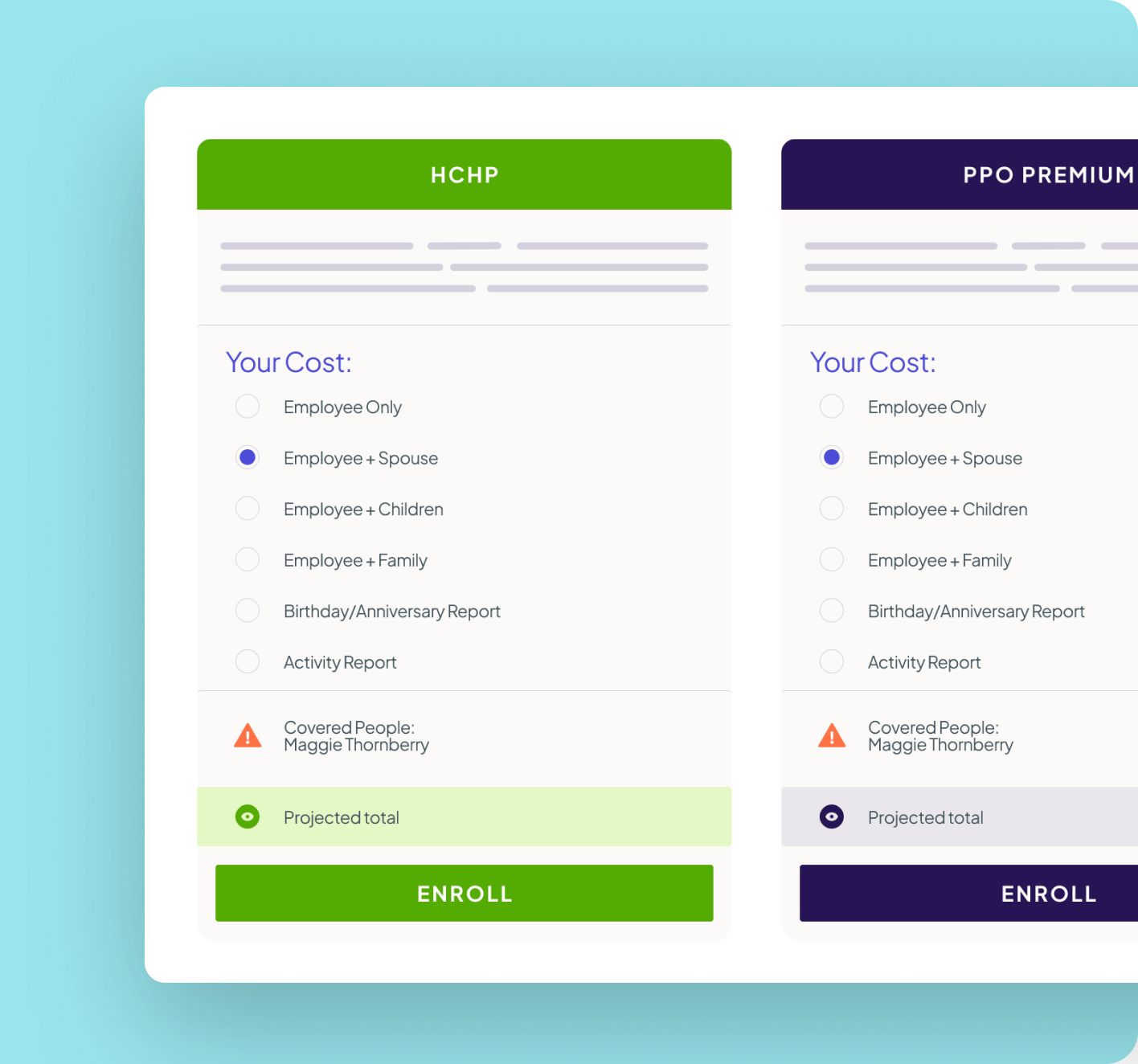
How Do I Manage Open Enrollment Without All The Chaos?
Tackle Open Enrollment with less stress.
The high-stakes Open Enrollment period often strains HR teams, revealing gaps in systems, communications, and employee understanding.
Employers want a smoother, more strategic process with fewer fire drills and better participation.
Common Challenges of Open Enrollment
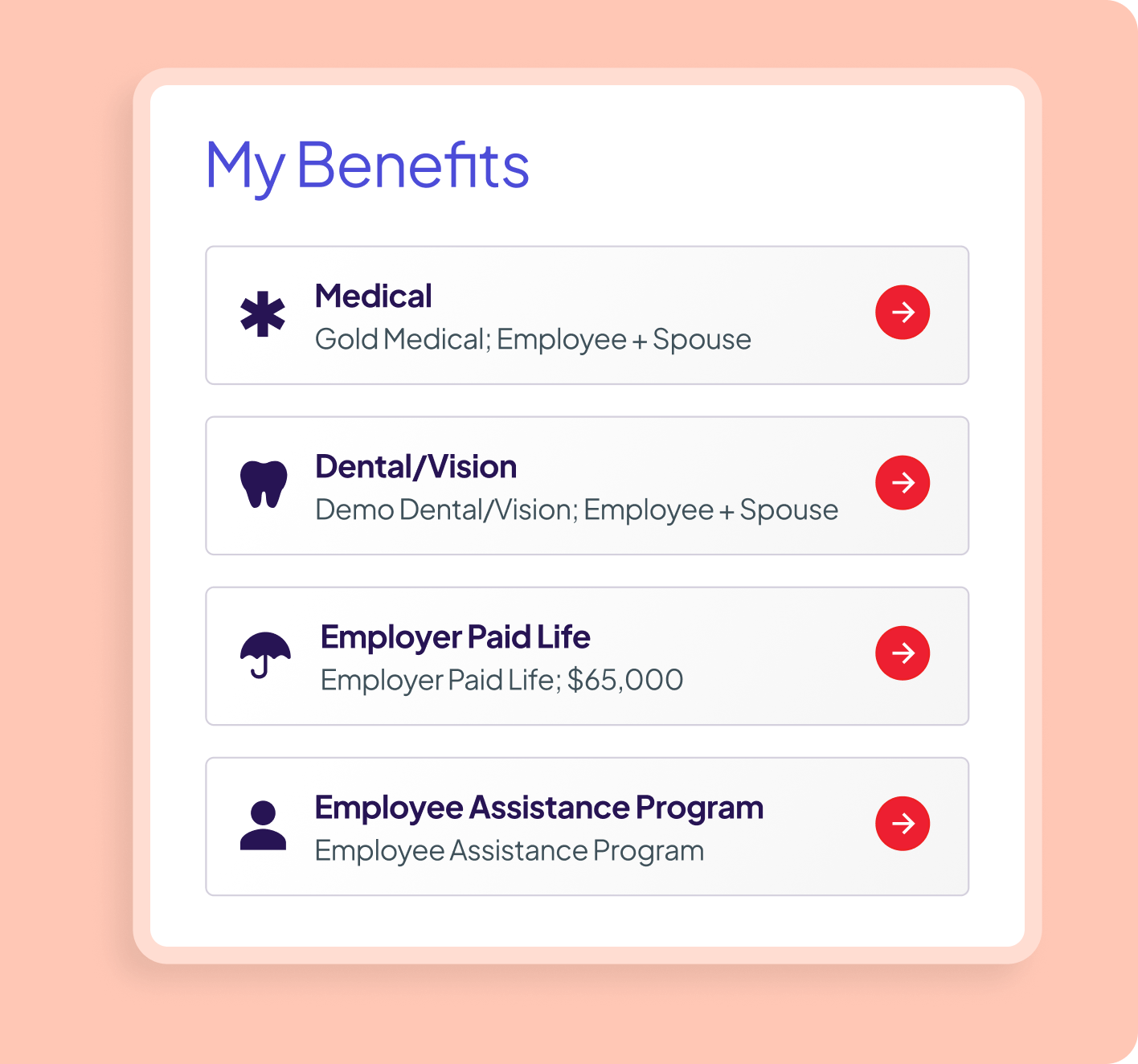
How Can We Increase Benefit Satisfaction?
Benefits only work if employees use them.
Participation and satisfaction gaps often come down to confusion, poor visibility, or a one-size-fits-all approach. Employees want relevant guidance. You want higher enrollment and better outcomes.

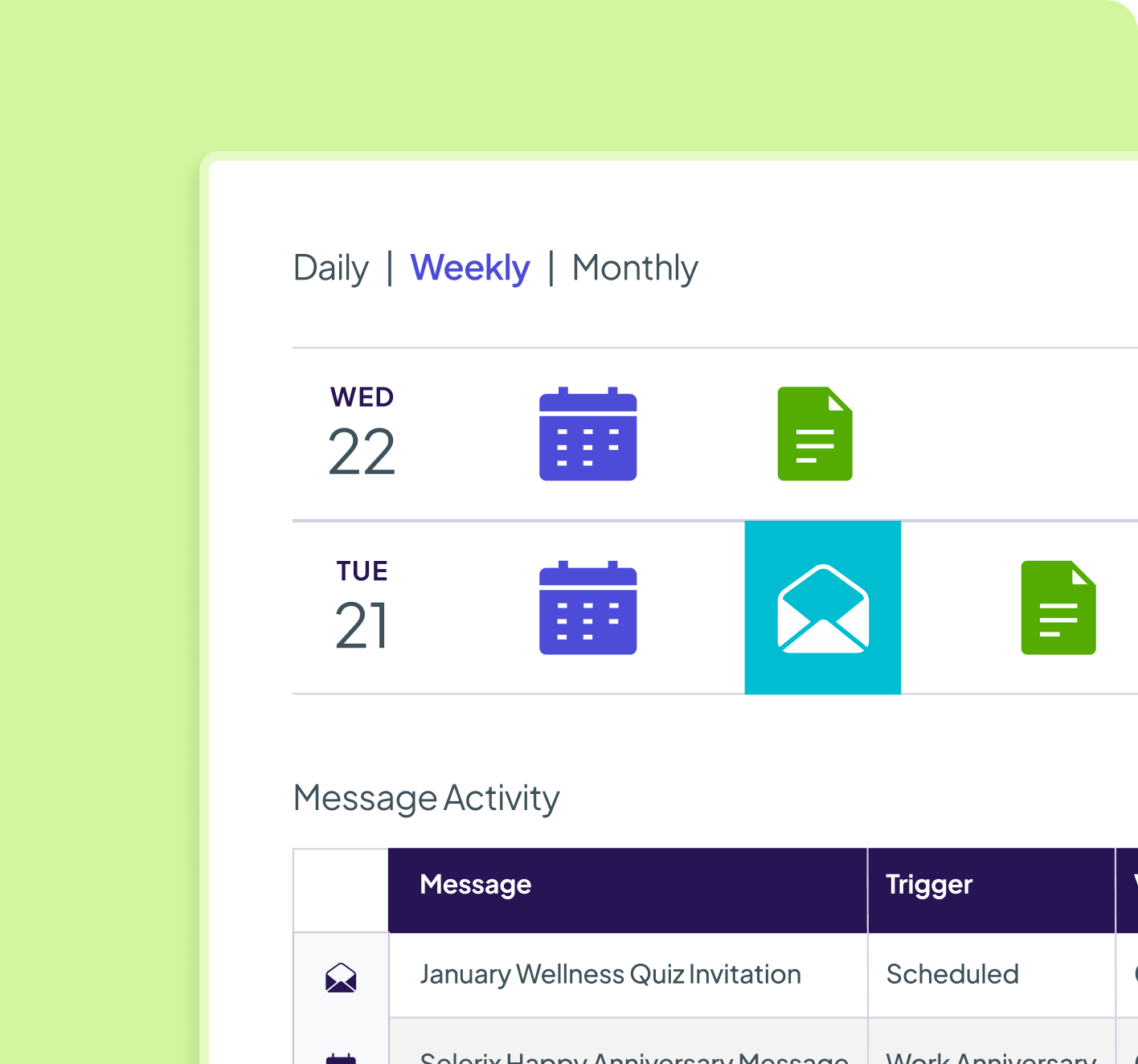
How Do We Improve Communication About Benefits?
Cut through the noise with timely, targeted communication.
Benefits details often get buried in inboxes or overlooked entirely. To engage employees, you need the right message, at the right time, on the right channel.

Hi Alex, your Open Enrollment window closes this Friday. Need help picking a plan? Click here to compare your options.
Congratulations on your new arrival, Jamie! Don’t forget — you have 30 days to add your baby to your benefits. Here’s how to get started!
When communication lives across too many platforms, it’s easy for critical benefits updates to get lost in the shuffle. Employees miss out—and HR teams struggle to keep everyone aligned.
How Do I Stay Compliant With ACA?
Keep your organization audit-ready, year-round.
ACA compliance requires accuracy, tracking, and timely reporting, but many employers struggle with scattered data or manual processes that invite risk.
What’s the Easiest Way to Manage COBRA?
Handle COBRA events with confidence and compassion.
Life happens — and when it does, employees count on COBRA to maintain coverage. HR teams need a consistent, compliant way to handle notifications, timelines, and eligibility without manual juggling.

Hi Jordan, since your coverage recently ended, you may be eligible for COBRA continuation. Here’s what to know and how to enroll if you choose to continue your benefits.
How Can We Make Benefits
Easier For New Hires?
Make a strong first impression with seamless onboarding.
New hires are often overwhelmed, and benefits enrollment is just one of many tasks they face. You need a clear, supportive process that helps them get started, without errors or delays.

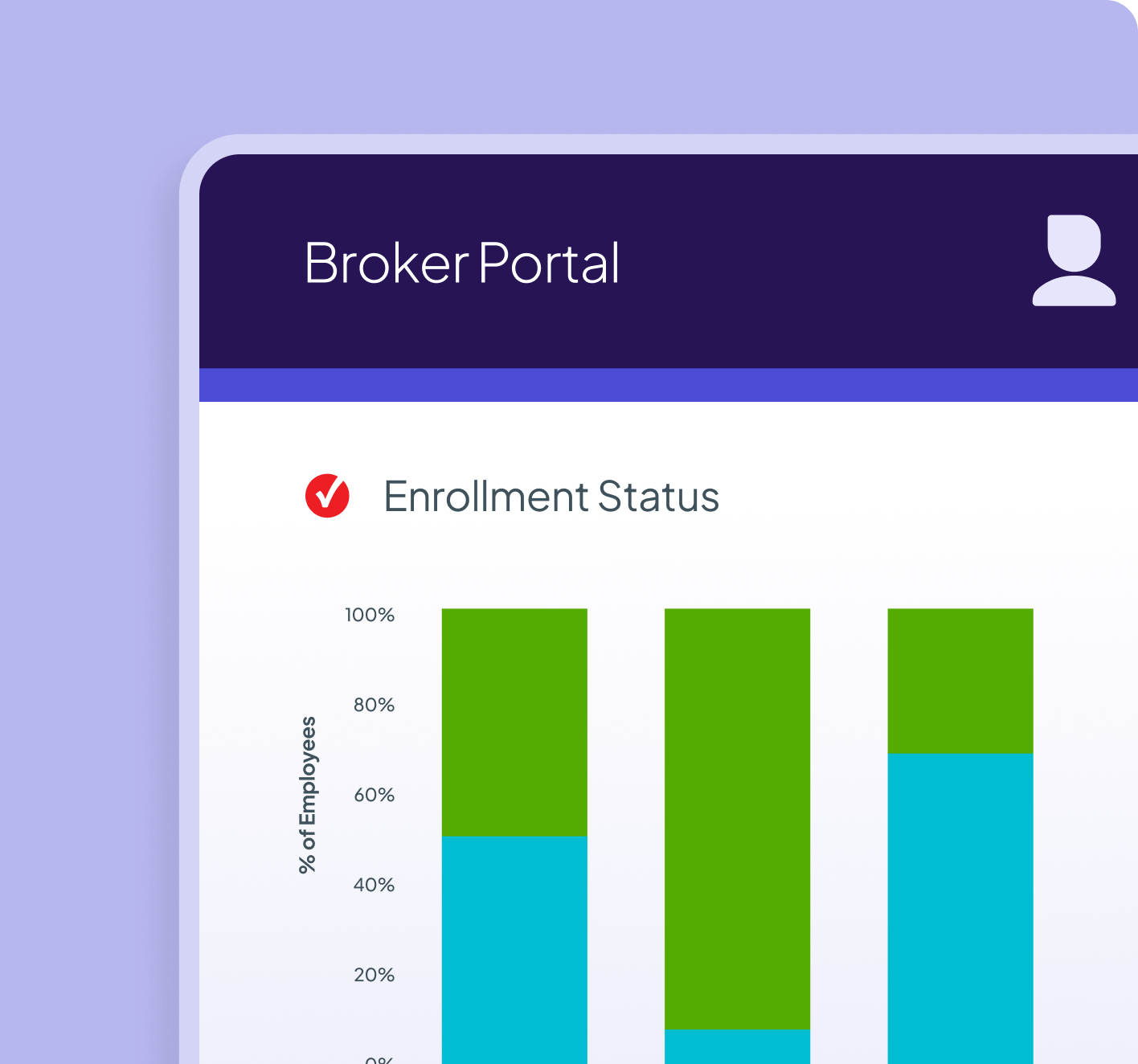
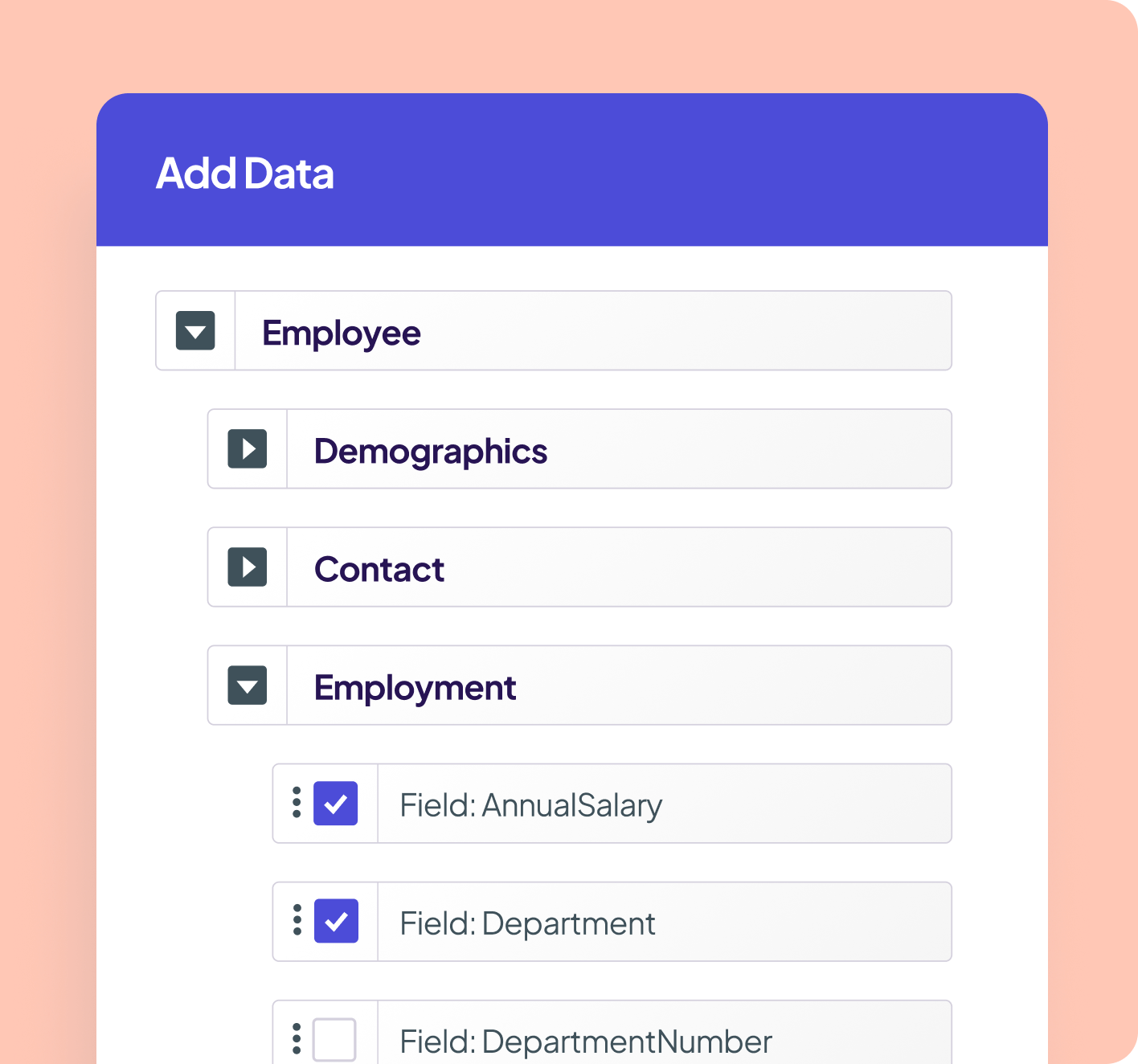
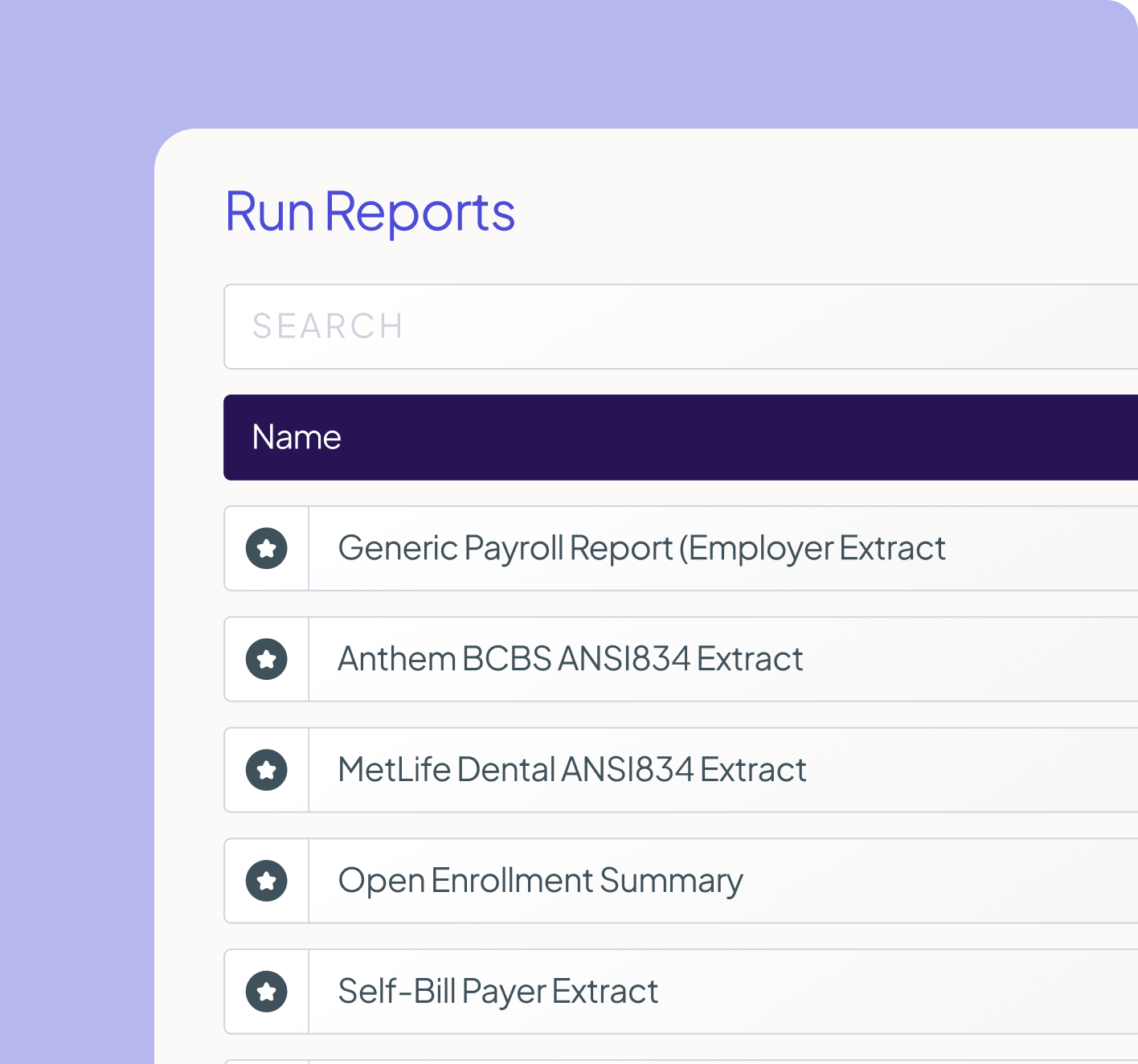
How Can We Improve Our Benefits Strategy?
Turn benefits data into smarter decisions.
You can’t fix what you can’t see. From participation trends to eligibility errors, employers need clear, timely insights to measure performance, identify gaps, and improve strategy.
Common reporting frustrations:
Too many platforms, not enough integration—leading to manual work and missed connections.
